Current Standards of Care Have Not Changed Significantly in Over 40 Years1-10
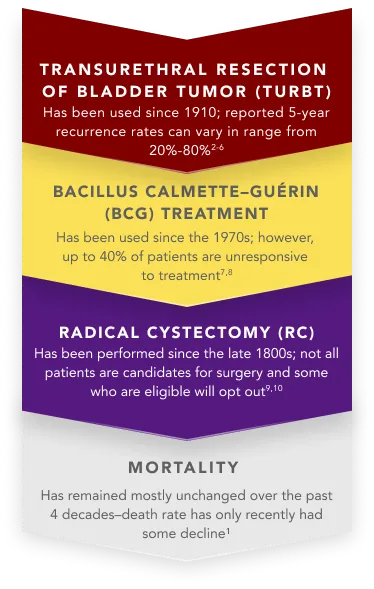
Widely Used Standard-Of-Care Treatment Options for NMIBC
BCG shortage
A shortage beginning in 2012 necessitated the use of alternative dosing and treatment considerations for patients with NMIBC.11

According to the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®), in the event of a shortage, BCG should be prioritized for high-risk induction patients.12
- Intravesical chemotherapy may be used as an alternative to BCG
- National Comprehensive Cancer Network® (NCCN®) provides recommendations for dose splitting/patient prioritization
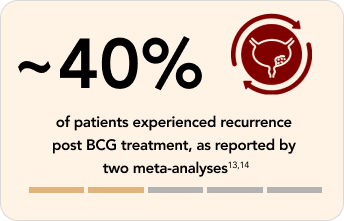
Clinical limitations of Bacillus Calmette–Guérin (BCG) treatment
Recurrence is likely in patients with NMIBC treated with intravesical BCG13,14
BCG unresponsiveness
BCG unresponsiveness indicates that a patient didn’t respond to an adequate dose of BCG therapy.15
Adequate BCG dosing is defined as the patient having completed at least 1 of the following16:
- Five of 6 doses of an initial induction course plus at least 2 of 3 doses of maintenance therapy
- Five of 6 doses of an initial induction course plus at least 2 of 6 doses of a second induction course
If a patient doesn’t respond after completing either of the above, it is determined that no further doses will be beneficial.15,16
The FDA defines BCG-unresponsive disease as being at least 1 of the following16:
- Persistent or recurrent carcinoma in situ (CIS) alone or with recurrent Ta/T1 (noninvasive papillary disease/tumor invades the subepithelial connective tissue) within 12 months of completion of adequate BCG treatment
- Recurrent high-grade Ta/T1 disease within 6 months of completion of adequate BCG treatment
References:
Cancer stat facts: bladder cancer. National Cancer Institute: Surveillance, Epidemiology, and End Results Program. Accessed February 13, 2024. https://seer.cancer.gov/statfacts/html/urinb.html
Joyce DD. Transurethral resection of bladder tumor: standard technique and new advancements. Published November 24, 2020. Accessed February 14, 2024. https://www.urologytimes.com/view/transurethral-resection-of-the-bladder-tumor-standard-technique-and-new-advancements
Sylvester RJ, van der Meijden AP, Oosterlinck W, et al. Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol. 2006;49(3):466-477. doi:10.1016/j.eururo.2005.12.031
Fernandez-Gomez J, Madero R, Solsona E, et al. Predicting nonmuscle invasive bladder cancer recurrence and progression in patients treated with Bacillus Calmette–Guerin: the CUETO scoring model. J Urol. 2009;182(5):2195-2203. doi:10.1016/j.juro.2009.07.016
Cambier S, Sylvester RJ, Collette L, et al. EORTC nomograms and risk groups for predicting recurrence, progression, and disease-specific and overall survival in non–muscle-invasive stage Ta-T1 urothelial bladder cancer patients treated with 1-3 years of maintenance Bacillus Calmette-Guérin. Eur Urol. 2016;69(1):60-69. doi:10.1016/j.eururo.2015.06.045
Martin-Doyle W, Leow JJ, Orsola A, Chang SL, Bellmunt J. Improving selection criteria for early cystectomy in high-grade T1 bladder cancer: a meta-analysis of 15,215 patients. J Clin Oncol. 2015;33(6):643-650. doi:10.1200/JCO.2014.57.6967
Jiang S, Redelman-Sidi G. BCG in bladder cancer immunotherapy. Cancers (Basel). 2022;14(13):3073. doi:10.3390/cancers14133073
Kodera A, Mohammed M, Lim P, Abdalla O, Elhadi M. The management of Bacillus Calmette-Guérin (BCG) failure in high-risk non-muscle invasive bladder cancer: a review article. Cureus. 2023;15(6):e40962. doi:10.7759/cureus.40962
Radical cystectomy. Medscape. Updated July 23, 2020. Accessed February 14, 2024. https://emedicine.medscape.com/article/448623-overview#a5
de Vere White R, Lara Jr PN, Black PC, Evans CP, Dall’Era M. Framing pragmatic strategies to reduce mortality from bladder cancer: an endorsement from the Society of Urologic Oncology. J Clin Oncol. 2020;38(16):1760-1762. doi:10.1200/JCO.19.01731
Implications of the national BCG drug shortage. End Drug Shortages Alliance. Published February 14, 2023. Accessed February 14, 2024. https://info.enddrugshortages.com/External/WCPages/WCWebContent/webcontentpage.aspx?ContentID=68
Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Bladder Cancer V3.2024. © National Comprehensive Cancer Network, Inc. 2024. All rights reserved. Accessed April 22, 2024. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
Böhle A, Jocham D, Bock PR. Intravesical bacillus Calmette-Guerin versus mitomycin C for superficial bladder cancer: a formal meta-analysis of comparative studies on recurrence and toxicity. J Urol. 2003;169(1):90-95. doi:10.1016/S0022-5347(05)64043-8
Han RF, Pan JG. Can intravesical bacillus Calmette-Guérin reduce recurrence in patients with superficial bladder cancer? A meta-analysis of randomized trials. Urology. 2006;67(6):1216-1223. doi:10.1016/j.urology.2005.12.014
Kim HS, Seo H K. Emerging treatments for bacillus Calmette–Guérin-unresponsive non-muscle-invasive bladder cancer. Investig Clin Urol. 2021;62(4):361-377. doi:10.4111/icu.20200602
BCG-unresponsive nonmuscle invasive bladder cancer: developing drugs and biologics for treatment guidance for industry. US Department of Health and Human Services. Food and Drug Administration. Published February 2018. Accessed February 14, 2024. https://www.fda.gov/media/101468/download
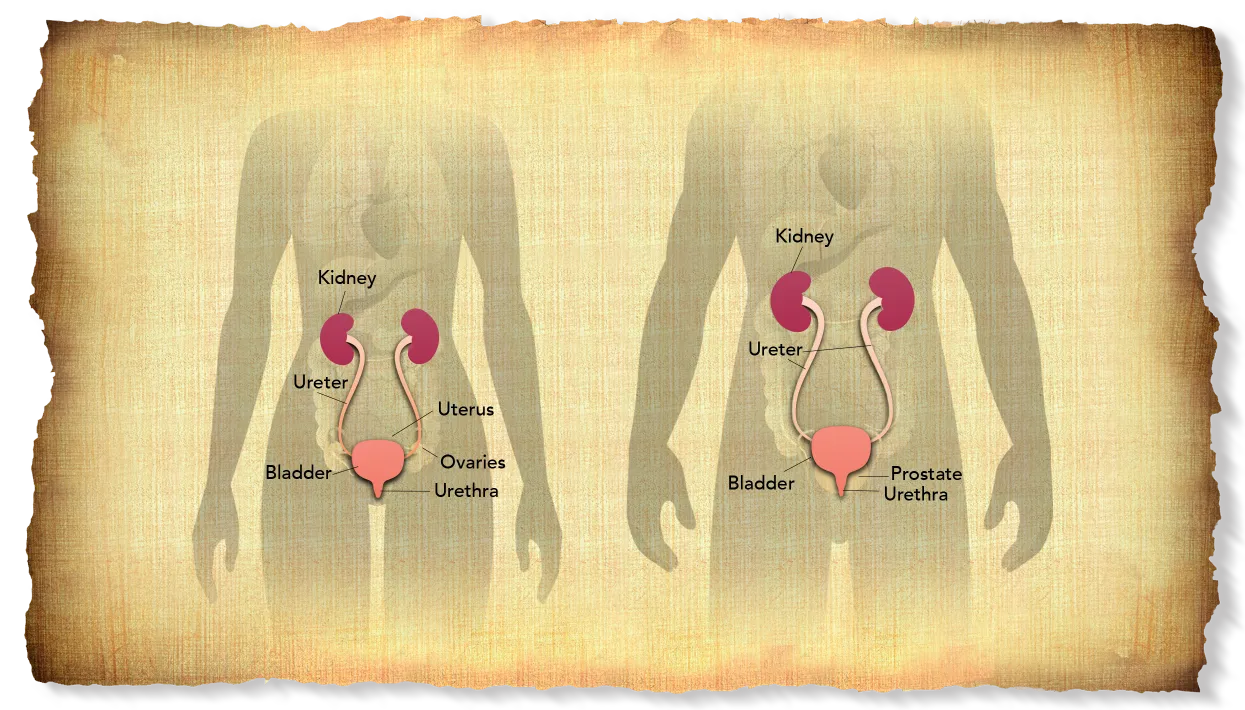
RC is the removal of the bladder, adjacent organs, and regional lymph nodes12
- In females, it can include the removal of the reproductive organs, such as ovaries, fallopian tubes, uterus, and anterior vagina, to achieve the best oncologic outcomes
- In males, it includes the removal of the prostate and the seminal vesicles
Patients require an alternative method to empty their bladder after RC. Options for urinary diversion include incontinent stoma (ileal conduit procedure), continent urinary reservoir catheterized by the patient, or a continent urinary reservoir connected to the urethra (orthotopic neobladder).13
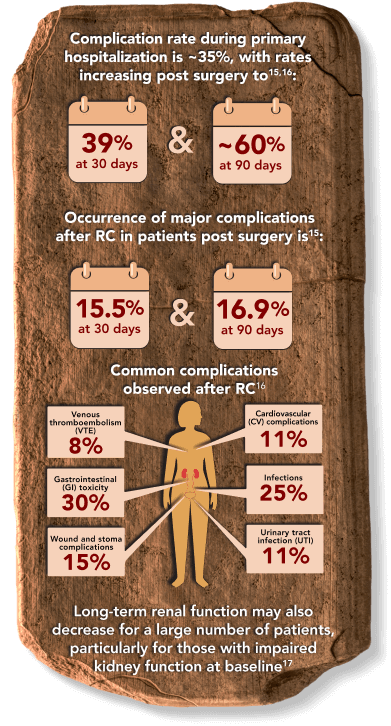
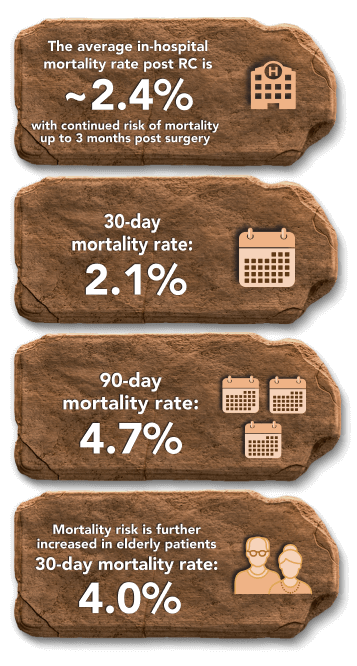
RC is associated with significant rates of complications and mortality14
Despite improvements in surgical technique and perioperative care, RC-associated complications continue to be an issue both during surgery and in the months that follow.
Mortality rates After RC15,18
RC can have long-term impact on patients13
The majority of patients deal with reduced health-related quality of life (HRQoL).13
- Patients receiving RC might have treatment-related comorbidities that impact their HRQoL and their daily lives post surgery13
- A study of 30 patients with MIBC who were recruited between 2011 and 2012 was conducted to evaluate the patients’ unmet needs during their illness trajectory. Half of patients reported difficulty with post-surgical recovery and almost half (~47%) reported difficulties related to medical complications. During survivorship (~6 months post-surgery), ~67% of patients reported difficulties in daily living, ~43% reported changes in sexual function, and ~33% reported emotional distress
- Treatments requiring patients to travel long distances can also be burdensome as the distance to care centers has been identified as a reason that patients may be undertreated10
References:
Cancer stat facts: bladder cancer. National Cancer Institute: Surveillance, Epidemiology, and End Results Program. Accessed February 13, 2024. https://seer.cancer.gov/statfacts/html/urinb.html
Joyce DD. Transurethral resection of bladder tumor: standard technique and new advancements. Published November 24, 2020. Accessed February 14, 2024. https://www.urologytimes.com/view/transurethral-resection-of-the-bladder-tumor-standard-technique-and-new-advancements
Sylvester RJ, van der Meijden AP, Oosterlinck W, et al. Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol. 2006;49(3):466-477. doi:10.1016/j.eururo.2005.12.031
Fernandez-Gomez J, Madero R, Solsona E, et al. Predicting nonmuscle invasive bladder cancer recurrence and progression in patients treated with Bacillus Calmette–Guerin: the CUETO scoring model. J Urol. 2009;182(5):2195-2203. doi:10.1016/j.juro.2009.07.016
Cambier S, Sylvester RJ, Collette L, et al. EORTC nomograms and risk groups for predicting recurrence, progression, and disease-specific and overall survival in non–muscle-invasive stage Ta-T1 urothelial bladder cancer patients treated with 1-3 years of maintenance Bacillus Calmette-Guérin. Eur Urol. 2016;69(1):60-69. doi:10.1016/j.eururo.2015.06.045
Martin-Doyle W, Leow JJ, Orsola A, Chang SL, Bellmunt J. Improving selection criteria for early cystectomy in high-grade T1 bladder cancer: a meta-analysis of 15,215 patients. J Clin Oncol. 2015;33(6):643-650. doi:10.1200/JCO.2014.57.6967
Jiang S, Redelman-Sidi G. BCG in bladder cancer immunotherapy. Cancers (Basel). 2022;14(13):3073. doi:10.3390/cancers14133073
Kodera A, Mohammed M, Lim P, Abdalla O, Elhadi M. The management of Bacillus Calmette-Guérin (BCG) failure in high-risk non-muscle invasive bladder cancer: a review article. Cureus. 2023;15(6):e40962. doi:10.7759/cureus.40962
Radical cystectomy. Medscape. Updated July 23, 2020. Accessed February 14, 2024. https://emedicine.medscape.com/article/448623-overview#a5
de Vere White R, Lara Jr PN, Black PC, Evans CP, Dall’Era M. Framing pragmatic strategies to reduce mortality from bladder cancer: an endorsement from the Society of Urologic Oncology. J Clin Oncol. 2020;38(16):1760-1762. doi:10.1200/JCO.19.01731
Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Bladder Cancer V3.2024. © National Comprehensive Cancer Network, Inc. 2024. All rights reserved. Accessed April 22, 2024. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
Aminoltejari K, Black PC. Radical cystectomy: a review of techniques, developments and controversies. Transl Androl Urol. 2020;9(6):3073-3081. doi:10.21037/tau.2020.03.23
Mohamed NE, Chaoprang HP, Hudson S, et al. Muscle invasive bladder cancer: examining survivors’ burden and unmet needs. J Urol. 2014;191(1):48-53. doi:10.1016/j.juro.2013.07.062
Yamada S, Abe T, Sazawa A, et al. Comparative study of postoperative complications after radical cystectomy during the past two decades in Japan: radical cystectomy remains associated with significant postoperative morbidities. Urol Oncol. 2022;40(1):11.e17-11.e25. doi:10.1016/j.urolonc.2021.09.005
Maibom SL, Joensen UN, Poulsen AM, Kehlet H, Brasso K, Røder MA. Short term morbidity and mortality following radical cystectomy: a systematic review. BMJ Open. 2021;11(4):e043266. doi:10.1136/bmjopen-2020-043266
Hladun T, Ratajczak J, Salagierski M. Can we lower the rates of cystectomy complications by modifying risk factors? A review of the literature. Cent European J Urol. 2022;75(1):28-34. doi:10.5173/ceju.2022.0292
Schmidt B, Velaer KN, Thomas IC, et al. Renal morbidity following radical cystectomy in patients with bladder cancer. Eur Urol Open Sci. 2022;35:29-36. doi:10.1016/j.euros.2021/11.001
Geiss R, Sebaste L, Valter R, et al. Complications and discharge after radical cystectomy for older patients with muscle-invasive bladder cancer: the ELCAPA-27 cohort study. Cancers (Basel). 2021;13(23):6010. doi:10.3390/cancers13236010